Next Generation PhD Health Data Scientists
We enable the brightest minds in health data science to become the research and innovation leaders of tomorrow
Our ambition
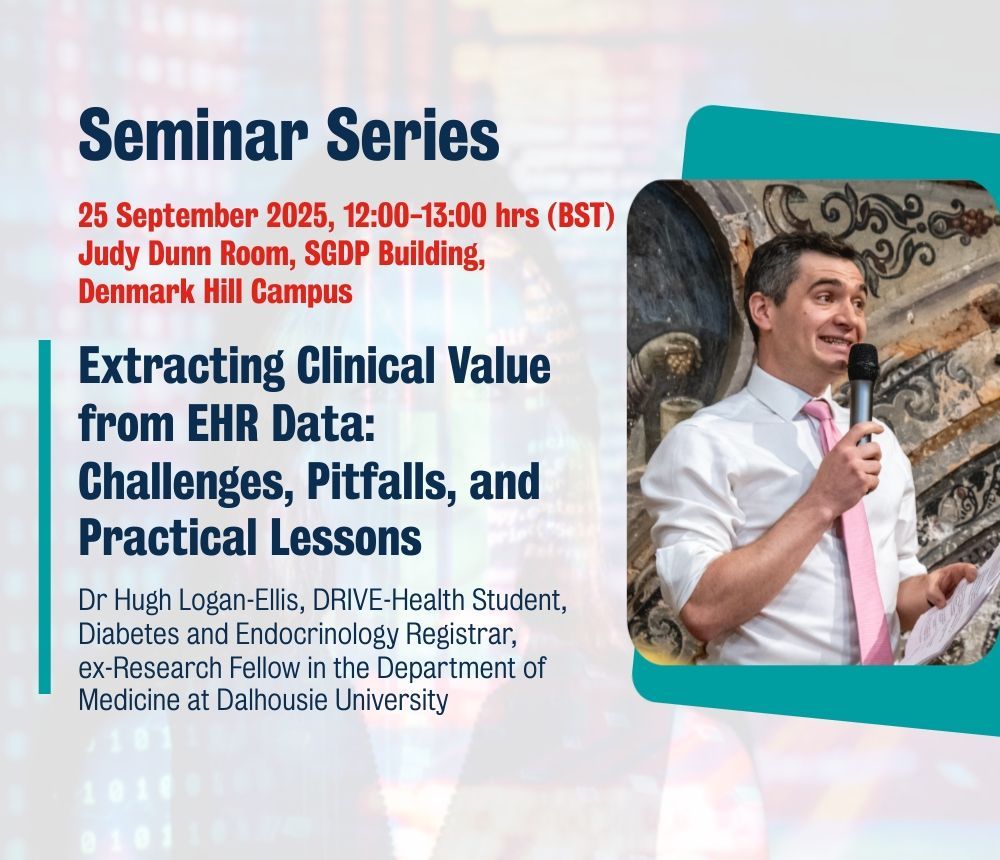
The King's College London Centre for Doctoral Training in Data-Driven Health (KCL DRIVE-Health) is training the next generation of PhD health data scientists to become the innovation leaders of tomorrow. Our students work within an active NHS environment, and develop new models of data-driven care, whilst leveraging significant recent investment and infrastructure in Health Data Research within the UK.
Our strategic aims
To provide world-class training in health data science research to the next generation of health data scientists, who will have the multidisciplinary skills needed to enable transformations in public health and breakthrough treatments

To solve the most challenging problems in data-driven health research, through a diverse community of the brightest minds in health data science; and an open, collaborative culture which fosters exchange and champions innovation
To co-create a translational cross-sector collaboration with the NHS, industry, enterprise, policy makers and academia - a first of it's kind for health informatics training in the UK. We work with our broad network of strategic partners to ensure that the UK health sciences sector remains at the global forefront of innovation
Our science and learning environment
There are significant opportunities to revolutionise the delivery of healthcare, with the growing availability of biological, social, genomic, imaging and sensor/Internet-of-Things datasets and electronic health records. The KCL DRIVE-Health PhD Programmes focus on four key scientific themes.
Latest News, Views & Insights